
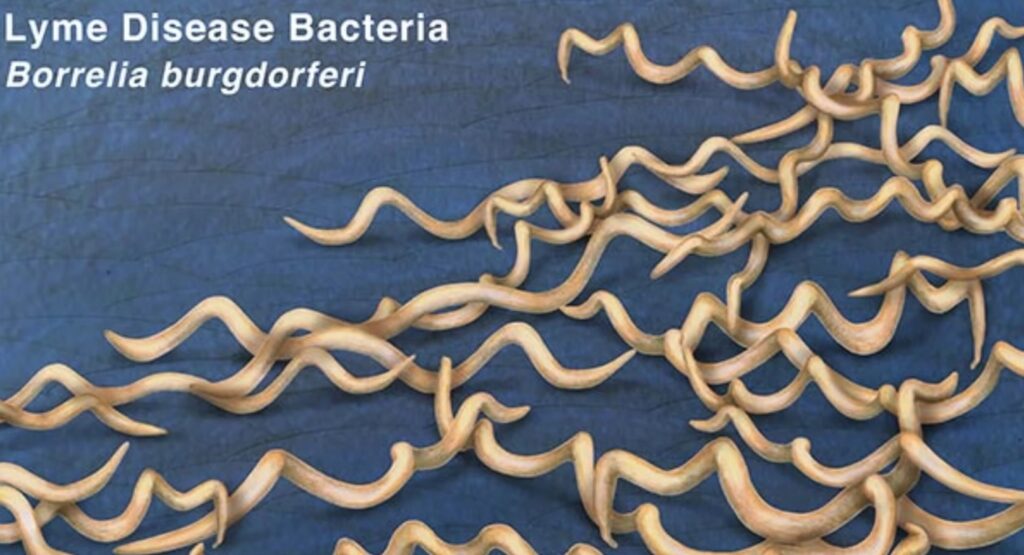
Lyme disease is a potentially serious bacterial infection caused by Borrelia burgdorferi, and less commonly Borrelia mayonii. These bacteria are transmitted to humans through the bite of an infected black-legged tick, commonly known as the deer tick (Ixodes scapularis). First identified in Lyme, Connecticut, in 1975, the disease has since become the most common vector-borne illness in the United States and parts of Europe.
According to the CDC, approximately 476,000 Americans are diagnosed and treated for Lyme disease annually, though only around 30,000 cases are officially reported. Early diagnosis and proper treatment are essential to avoid long-term complications.
Where Is Lyme Disease Most Common?

Ticks that carry Borrelia bacteria are found across North America, Europe, and Asia, but Lyme disease is most common in:
- Northeastern U.S. (New York, Massachusetts, Connecticut, Pennsylvania)
- Upper Midwest (Wisconsin, Minnesota)
- Mid-Atlantic states
- South-central and southeastern Canada
- Parts of Central and Northern Europe
You’re most at risk during spring and summer, when ticks are active, especially if you spend time in wooded, grassy, or brushy areas.
Stages and Symptoms of Lyme Disease
Lyme disease symptoms evolve over three stages, which may overlap or progress unpredictably. Some people may not exhibit symptoms until the later stages.
Stage 1: Early Localized Lyme Disease (3–30 Days Post-Bite)
This early phase typically involves:
- Erythema Migrans (EM) Rash
- Occurs in 70–80% of infected individuals
- Appears as a bull’s-eye rash (red ring with central clearing)
- Expands slowly and may feel warm but isn’t usually painful or itchy
- May grow up to 12 inches or more
- Flu-like Symptoms
- Fever
- Chills
- Headache
- Fatigue
- Muscle and joint aches
- Swollen lymph nodes
Stage 2: Early Disseminated Lyme Disease (Weeks to Months Post-Bite)
If untreated, the infection can spread, leading to:
- Multiple EM rashes on the body
- Facial palsy (Bell’s palsy) or muscle weakness
- Neck stiffness or meningitis
- Irregular heartbeat or Lyme carditis
- Pain/numbness in hands, legs, or back
- Blurred vision or eye inflammation
Stage 3: Late Disseminated Lyme Disease (Months to Years Post-Bite)
In the absence of treatment, the bacteria can affect major systems:
- Chronic arthritis—especially in large joints like the knees
- Cognitive problems, such as memory issues, difficulty concentrating (“brain fog”)
- Peripheral neuropathy (numbness, tingling, or burning)
- Acrodermatitis chronica atrophicans (European variant): Skin thinning and discoloration on hands, feet, or joints
How is Lyme Disease Diagnosed?
Diagnosis is based on:
- Symptom review
- Known exposure to ticks
- Physical signs, especially EM rash
- Blood tests:
- Enzyme-linked immunosorbent assay (ELISA)
- Western blot test (confirmation test)
Note: Blood tests are more reliable a few weeks after infection. Early testing may give false negatives.
Treatment Options for Lyme Disease
1. Antibiotics (Standard Treatment)
Early Lyme disease is effectively treated with oral antibiotics:
- Doxycycline (for most adults and children over 8)
- Amoxicillin or Cefuroxime (for pregnant individuals and younger children)
Duration: Typically 10–14 days, up to 21 days in some cases.
2. Intravenous (IV) Antibiotics
Required for severe cases involving:
- Neurological symptoms
- Heart abnormalities (Lyme carditis)
- Chronic arthritis
3. Post-Treatment Lyme Disease Syndrome (PTLDS)
Some people continue to experience fatigue, joint pain, or mental fog after completing treatment. This is not due to ongoing infection, and long-term antibiotics are not effective. Research suggests PTLDS may be caused by:
- Autoimmune responses
- Tissue damage from initial infection
What to Do if a Tick Bites You
Step-by-Step Tick Removal:
- Use fine-tipped tweezers to grasp the tick as close to the skin as possible.
- Pull upward steadily—don’t twist or jerk.
- Clean the area with soap and water, then disinfect with alcohol.
- Save the tick in a sealed bag with the date in case you develop symptoms later.
- Don’t use petroleum jelly, nail polish, heat, or bare fingers to remove a tick.
Preventive Antibiotics
In some high-risk cases, a single dose of doxycycline may be prescribed as a preventive measure—only if:
- The tick is confirmed to be a deer tick
- It was attached for 36+ hours
- Prophylaxis is given within 72 hours of removal
Prevention: How to Reduce Your Risk of Lyme Disease
Avoid Tick Habitats:
- Stay on clear trails
- Avoid tall grasses, leaf litter, and dense woods
Wear Protective Clothing:
- Long sleeves and pants tucked into socks
- Light-colored clothing to spot ticks easily
Use Tick Repellents:
- Apply DEET (≥20%) on skin
- Treat clothing with permethrin
Tick Checks and Hygiene:
- Shower within 2 hours of coming indoors
- Check under arms, behind knees, around ears, scalp, and groin
- Inspect pets and gear
FAQs About Lyme Disease
Is Lyme Disease Contagious?
No. Lyme disease cannot be transmitted from person to person.
Can Lyme Disease Be Fatal?
Rarely. Complications like Lyme carditis can be serious but are treatable if caught early.
Can Pets Get Lyme Disease?
Yes. Dogs are especially susceptible and should be protected with tick preventives.
Conclusion: Early Action is Key to Beating Lyme Disease
Lyme disease is a preventable and treatable illness, but awareness is your first defense. Recognizing the signs and taking quick action after a tick bite can prevent the progression to more serious stages. If you’ve spent time in areas where deer ticks live and start to notice symptoms, consult a healthcare provider promptly. With early antibiotic treatment, most people recover fully and quickly.